
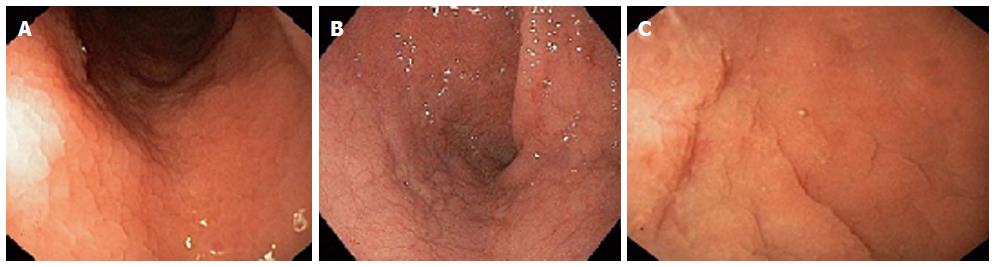
Testing at-risk individuals is strongly recommended to detect cases before substantial morbidity develops. Coeliac disease can be present despite negative coeliac disease serology, but this is uncommon and excluding other causes of villous atrophy (see below) is important. 3,6Ĭorrelation of histology and serology with clinical history is important. disease remission confirmed by symptom resolution, normalised coeliac disease serology and, most reliably and importantly, mucosal healing following treatment with a GFD.intestinal histology showing raised intraepithelial lymphocytes (>25 per 100 enterocytes), crypt hyperplasia and villous atrophy (Figure 1).In patients with positive coeliac disease serology, the diagnosis is confirmed by the presence of characteristic small intestinal mucosal changes. In clinical practice, suspected patients are generally screened with coeliac disease serology. 5 As expeditious diagnosis and treatment with a strict, lifelong gluten-free diet (GFD) minimises long-term complications, 3 application of the appropriate tests to ensure accurate diagnosis and follow-up is crucial.

However, its broad and often subtle presentation makes detection challenging, and means 80% of Australians with coeliac disease remain undetected. 3 As 1.5% of Australians have coeliac disease, it is one of the most common autoimmune illnesses that general practitioners (GPs) will encounter.

2–4 Mortality is increased because of lymphoproliferative malignancy, sepsis and refractory disease. 1 Untreated disease reduces quality of life, increases healthcare use and is associated with substantial morbidity.
#Celiac endoscopy findings series
Articles in this series aim to provide information about emerging laboratory tests that general practitioners may encounter.Ĭoeliac disease is an immune illness, triggered by dietary gluten, that causes a broad range of gastrointestinal and extra-intestinal manifestations. This article is the second in a series on pathology testing.


 0 kommentar(er)
0 kommentar(er)
